For years, it has been a widely held notion that individuals who engage in excessive, strenuous physical activities, such as running, are likely to develop osteoarthritis affecting the knees or the hip, medical experts say. This has been attributed to increased stress and impact that weight-bearing joints in the body may sustain from the high-impact exercise. A recent study, however, offers a different vantage point to this long-standing view, claiming that runners stand at a lower risk of developing osteoarthritis and eventually requiring hip replacement surgery for the joint disease than people who choose walking as their primary exercise.
Paul Williams, an exercise epidemiologist at Berkeley Lab’s Life Sciences Division, reportedly set out on a study that zeroed in on how running and walking may affect a person’s risk of osteoarthritis and hip replacement. The recent study involved nearly 90,000 participants, 74,752 of whom were runners, while 14,625 were walkers. After following both groups for an average of seven years, more than 2000 runners reportedly received diagnosis of osteoarthritis, while over 250 of them went through hip replacement surgery. On the other hand, nearly 700 walkers were diagnosed with the arthritic condition and more than 100 have also gone through hip replacement.
Study results reportedly suggest that volunteers who ran more than one mile each day showed a 15 percent decreased risk of osteoarthritis and 35 percent lower hip replacement risk, compared to individuals who lead a sedentary lifestyle. No significant changes have been observed even in runners who ran at higher mileages or participated in multiple marathons in a single year. While other factors may have also played a role, findings also reportedly revealed that running may have significantly contributed to low osteoarthritis and hip replacement risk due, in part, to the physical activity’s connection to lower body mass index.
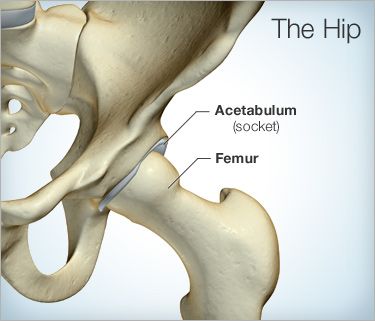
Osteoarthritis is a joint disorder which usually results from the progressive breakdown of the protective cartilage in joints, as was described by medical journals. Also known as “wear and tear” arthritis, osteoarthritis has reportedly taken an increasing role in prevalence, affecting 20 million people from the American population alone, according to government statistics reports. Individuals who may have developed the arthritic condition particularly in the hip may experience pain, stiffness, and limited mobility, making regular, day-to-day activities difficult to perform and causing a major impact to their quality of life.
Hip replacement surgery, also referred to as total hip replacement, has been the medical recourse of most patients whose osteoarthritis in the hip has progressed, according to health experts. It is a surgical procedure that involves the removal and replacement of a severely damaged hip joint with an artificial component known as prosthesis or hip replacement implants. Medical experts point out, however, that hip replacement surgery is only recommended to patients whose symptoms of osteoarthritis have become severe that non-invasive treatments no longer suffice to provide relief.
Paul Williams, an exercise epidemiologist at Berkeley Lab’s Life Sciences Division, reportedly set out on a study that zeroed in on how running and walking may affect a person’s risk of osteoarthritis and hip replacement. The recent study involved nearly 90,000 participants, 74,752 of whom were runners, while 14,625 were walkers. After following both groups for an average of seven years, more than 2000 runners reportedly received diagnosis of osteoarthritis, while over 250 of them went through hip replacement surgery. On the other hand, nearly 700 walkers were diagnosed with the arthritic condition and more than 100 have also gone through hip replacement.
Study results reportedly suggest that volunteers who ran more than one mile each day showed a 15 percent decreased risk of osteoarthritis and 35 percent lower hip replacement risk, compared to individuals who lead a sedentary lifestyle. No significant changes have been observed even in runners who ran at higher mileages or participated in multiple marathons in a single year. While other factors may have also played a role, findings also reportedly revealed that running may have significantly contributed to low osteoarthritis and hip replacement risk due, in part, to the physical activity’s connection to lower body mass index.
Osteoarthritis is a joint disorder which usually results from the progressive breakdown of the protective cartilage in joints, as was described by medical journals. Also known as “wear and tear” arthritis, osteoarthritis has reportedly taken an increasing role in prevalence, affecting 20 million people from the American population alone, according to government statistics reports. Individuals who may have developed the arthritic condition particularly in the hip may experience pain, stiffness, and limited mobility, making regular, day-to-day activities difficult to perform and causing a major impact to their quality of life.
Hip replacement surgery, also referred to as total hip replacement, has been the medical recourse of most patients whose osteoarthritis in the hip has progressed, according to health experts. It is a surgical procedure that involves the removal and replacement of a severely damaged hip joint with an artificial component known as prosthesis or hip replacement implants. Medical experts point out, however, that hip replacement surgery is only recommended to patients whose symptoms of osteoarthritis have become severe that non-invasive treatments no longer suffice to provide relief.